PHYSICAL HEALTH
Being overweight or obese increases your chances of dying from hypertension,
2 diabetes,
Coronary heart disease,
Stroke,
Gallbladder disease,
Osteoarthritis,
Sleep apnea,
Respiratory problems,
Dyslipidemia and endometrial,
Breast, prostate and colon cancers.
Overweight;
Obesity is a medical condition, sometimes considered a disease, in which excess body fat has accumulated to such an extent that it can potentially have negative effects on health
Symptoms;
Increased fats.
Excessive weights of body
Cure:
Physical work.
Walk
Exercise
Healthy diet.
Intake of water.
On the most basic level, obesity happens when you consume more calories than your body can use. Many things may play a role in why you may eat more food than your body needs:
Eating habits: Consuming more calories than your body needs, eating ultra-processed food, high-sugar foods and drinks, and foods with high amounts of saturated fat may cause overweight.
Genetics: people with obesity carry specific genes (obesity-susceptibility genes) that affect appetite. It’s not clear if people with overweight have the same genetic makeup.
Lack of physical activity: High amounts of screen time — like watching TV, playing video games or spending time on your mobile phone or laptop — cut into the time you have for physical activity.
Lack of sleep: Missing out on at least seven hours of sleep can affect the hormones that keep hunger urges under control.
Stress: Your brain and body react to stress by making more hormones like
Cortisol that manage hunger. When you’re stressed, you’re more likely to eat high-fat, high-sugar food (comfort food) that your body stores as extra fat.
Diabetes, a chronic condition, is diagnosed and monitored with blood glucose level.
Chronic disease that occurs either when the pancreas does not produce enough insulin or when the body cannot effectively use the insulin it produces. Insulin is a hormone that regulates blood glucose.
Symptoms: Frequent urination; increased thirst; increased hunger.
Treatment: Lifestyle changes; Diabetes medication;
Complications: Metabolic imbalances; cardiovascular diseases; Nerve and brain damage; Kidney failure; gastrointestinal changes;
Coronary artery disease, also called coronary heart disease, ischemic heart disease, myocardial ischemia, or simply heart disease, involves the reduction of blood flow to the cardiac muscle due to build-up of atherosclerotic plaque in the arteries of the heart. It is the most common of the cardiovascular diseases.
TYPES:
- Obstructive coronary artery disease.
- Nonconstructive coronary artery disease.
- Spontaneous coronary artery dissection.
Coronary heart disease is a disease of the blood vessels supplying the heart muscle. Cardiovascular diseases are the leading cause of death.
Symptoms of coronary artery disease happen when the heart doesn’t get enough oxygen-rich blood. Coronary artery disease symptoms may include:
Chest pain, called angina. You may feel squeezing, pressure, heaviness, tightness or pain in the chest. It may feel like somebody is standing on your chest. The chest pain usually affects the middle or left side of the chest.
- Shortness of breath. You may feel like you can’t catch your breath.
- Fatigue. If the heart can’t pump enough blood to meet your body’s needs, you may feel unusually tired.
A completely blocked coronary artery will cause a heart attack. Common heart attack symptoms include:
- Chest pain that may feel like pressure, tightness, squeezing or aching.
- Pain or discomfort that spreads to the shoulder, arm, back, neck, jaw, teeth or sometimes the upper belly.
- Cold sweats.
- Coronary artery disease is caused by the buildup of fats, cholesterol and other substances in and on the walls of the heart arteries
Some causes of atherosclerosis and coronary artery disease are:
- Diabetes or insulin resistance.
- High blood pressure.
- Lack of exercise.
Some causes of atherosclerosis and coronary artery disease are:
- Diabetes or insulin resistance.
- High blood pressure.
- Lack of exercise.
Stroke
A stroke happens when blood flow to your brain is stopped. It is an emergency situation. It can be caused by a narrowed blood vessel, bleeding, or a clot that blocks blood flow. Symptoms can happen suddenly.
Signs of a stroke, remember to think BE FAST:
- 1. Be watchful for a sudden loss of balance.
- 2:look out for sudden loss of vision in one or both eyes. Are they experiencing double vision?
- 3. Ask the person to smile. Look for a droop on one or both sides of their face, which is a sign of muscle weakness or paralysis.
- 4. A person having a stroke often has muscle weakness on one side. Ask them to raise their arms. If they have one-sided weakness (and didn’t have it before), one arm will stay higher while the other will sag and drop downward.
- 5 Strokes often cause a person to lose their ability to speak. They might slur their speech or have trouble choosing the right words.
- 6. Time is critical, so don’t wait to get help! If possible, look at your watch or a clock and remember when symptoms start. Telling a healthcare provider when symptoms started can help the provider know what treatment options are best for you.
What are the types of stroke?
There are two main ways that strokes can happen: ischemia and hemorrhage.
Ischemic stroke
Ischemia (pronounced “iss-key-me-uh”) is when cells don’t get enough blood flow to supply them with oxygen.
- Formation of a clot in your brain (thrombosis).
- A fragment of a clot that formed elsewhere in your body that breaks free and travels through your blood vessels until it gets stuck in your brain (embolism).
- Small vessel blockage (lacunar stroke), which can happen when you have long-term, untreated high blood pressure (hypertension), high cholesterol (hyperlipidemia) or high blood sugar (Type 2 diabetes).
- Unknown reasons (these are cryptogenic strokes; the word “cryptogenic” means
Hemorrhagic (pronounced “hem-or-aj-ick”) strokes cause bleeding in or around your brain. This happens in one of two ways:
- Bleeding inside of your brain (intracerebral). This happens when a blood vessel inside of your brain tears or breaks open, causing bleeding that puts pressure on the surrounding brain tissue.
- Bleeding into the subarachnoid space (the space between your brain and its outer covering). The arachnoid membrane, a thin layer of tissue with a spider web-like pattern on it, surrounds your brain. The space between it and your brain is the subarachnoid space (“sub” means “under”). Damage to blood vessels that pass through the arachnoid membrane can cause a subarachnoid hemorrhage, which is bleeding into the subarachnoid space, putting pressure on the brain tissue underneath.
Symptoms;
Increased fats.
Excessive weights of body
Cure:
Physical work.
Walk
Exercise
Healthy diet.
Intake of water.
On the most basic level, obesity happens when you consume more calories than your body can use. Many things may play a role in why you may eat more food than your body needs:
Eating habits: Consuming more calories than your body needs, eating ultra-processed food, high-sugar foods and drinks, and foods with high amounts of saturated fat may cause overweight.
Genetics: people with obesity carry specific genes (obesity-susceptibility genes) that affect appetite. It’s not clear if people with overweight have the same genetic makeup.
Lack of physical activity: High amounts of screen time — like watching TV, playing video games or spending time on your mobile phone or laptop — cut into the time you have for physical activity.
Lack of sleep: Missing out on at least seven hours of sleep can affect the hormones that keep hunger urges under control.
Stress: Your brain and body react to stress by making more hormones like
Cortisol that manage hunger. When you’re stressed, you’re more likely to eat high-fat, high-sugar food (comfort food) that your body stores as extra fat.
Diabetes, a chronic condition, is diagnosed and monitored with blood glucose level.
Chronic disease that occurs either when the pancreas does not produce enough insulin or when the body cannot effectively use the insulin it produces. Insulin is a hormone that regulates blood glucose.
Symptoms: Frequent urination; increased thirst; increased hunger.
Treatment: Lifestyle changes; Diabetes medication;
Complications: Metabolic imbalances; cardiovascular diseases; Nerve and brain damage; Kidney failure; gastrointestinal changes;
Coronary artery disease, also called coronary heart disease, ischemic heart disease, myocardial ischemia, or simply heart disease, involves the reduction of blood flow to the cardiac muscle due to build-up of atherosclerotic plaque in the arteries of the heart. It is the most common of the cardiovascular diseases.
TYPES:
- Obstructive coronary artery disease.
- Nonconstructive coronary artery disease.
- Spontaneous coronary artery dissection.
Coronary heart disease is a disease of the blood vessels supplying the heart muscle. Cardiovascular diseases are the leading cause of death.
Symptoms of coronary artery disease happen when the heart doesn’t get enough oxygen-rich blood. Coronary artery disease symptoms may include:
Chest pain, called angina. You may feel squeezing, pressure, heaviness, tightness or pain in the chest. It may feel like somebody is standing on your chest. The chest pain usually affects the middle or left side of the chest.
- Shortness of breath. You may feel like you can’t catch your breath.
- Fatigue. If the heart can’t pump enough blood to meet your body’s needs, you may feel unusually tired.
A completely blocked coronary artery will cause a heart attack. Common heart attack symptoms include:
- Chest pain that may feel like pressure, tightness, squeezing or aching.
- Pain or discomfort that spreads to the shoulder, arm, back, neck, jaw, teeth or sometimes the upper belly.
- Cold sweats.
- Coronary artery disease is caused by the buildup of fats, cholesterol and other substances in and on the walls of the heart arteries
Some causes of atherosclerosis and coronary artery disease are:
- Diabetes or insulin resistance.
- High blood pressure.
- Lack of exercise.
Some causes of atherosclerosis and coronary artery disease are:
- Diabetes or insulin resistance.
- High blood pressure.
- Lack of exercise.
Stroke
A stroke happens when blood flow to your brain is stopped. It is an emergency situation. It can be caused by a narrowed blood vessel, bleeding, or a clot that blocks blood flow. Symptoms can happen suddenly.
Signs of a stroke, remember to think BE FAST:
- 1. Be watchful for a sudden loss of balance.
- 2:look out for sudden loss of vision in one or both eyes. Are they experiencing double vision?
- 3. Ask the person to smile. Look for a droop on one or both sides of their face, which is a sign of muscle weakness or paralysis.
- 4. A person having a stroke often has muscle weakness on one side. Ask them to raise their arms. If they have one-sided weakness (and didn’t have it before), one arm will stay higher while the other will sag and drop downward.
- 5 Strokes often cause a person to lose their ability to speak. They might slur their speech or have trouble choosing the right words.
- 6. Time is critical, so don’t wait to get help! If possible, look at your watch or a clock and remember when symptoms start. Telling a healthcare provider when symptoms started can help the provider know what treatment options are best for you.
What are the types of stroke?
There are two main ways that strokes can happen: ischemia and hemorrhage.
Ischemic stroke
Ischemia (pronounced “iss-key-me-uh”) is when cells don’t get enough blood flow to supply them with oxygen.
- Formation of a clot in your brain (thrombosis).
- A fragment of a clot that formed elsewhere in your body that breaks free and travels through your blood vessels until it gets stuck in your brain (embolism).
- Small vessel blockage (lacunar stroke), which can happen when you have long-term, untreated high blood pressure (hypertension), high cholesterol (hyperlipidemia) or high blood sugar (Type 2 diabetes).
- Unknown reasons (these are cryptogenic strokes; the word “cryptogenic” means
Hemorrhagic (pronounced “hem-or-aj-ick”) strokes cause bleeding in or around your brain. This happens in one of two ways:
- Bleeding inside of your brain (intracerebral). This happens when a blood vessel inside of your brain tears or breaks open, causing bleeding that puts pressure on the surrounding brain tissue.
- Bleeding into the subarachnoid space (the space between your brain and its outer covering). The arachnoid membrane, a thin layer of tissue with a spider web-like pattern on it, surrounds your brain. The space between it and your brain is the subarachnoid space (“sub” means “under”). Damage to blood vessels that pass through the arachnoid membrane can cause a subarachnoid hemorrhage, which is bleeding into the subarachnoid space, putting pressure on the brain tissue underneath.
- What is gallbladder disease?
- Cholecystitis (inflammation of the gallbladder)
- Gallstones.
- Chronic calculous gallbladder disease (in which the natural movements needed to empty the gallbladder do not work well)
- Gangrene or abscesses.
- Growths of tissue in the gallbladder.
- Congenital defects of the gallbladder.
- Gallbladder disease refers to any condition that affects the health of your gallbladder. Your gallbladder is a small organ in your digestive system. It stores some of the bile your liver makes and sends it to your small intestine to help break down food there. It does this through a series of pipes called bile ducts.
Gallstones (cholelithiasis).
-
Gallstones
develop when excess bile products in your gallbladder — usually cholesterol — accumulate into lumps, which can continue to grow and accumulate. You can have gallstones without symptoms and never know they are there.
Cholecystitis (inflammation).
cholecystitis (inflammation) can be a sign of an infection or blockage of the gallbladder, a functional obstruction or, more rarely, cancer.
Biliary dyskinesia.
A functional motility problem has the same effects as a gallstone or other obstruction in your gallbladder or bile ducts. It causes bile to back up in your gallbladder, leading to chronic inflammation. But in this case, it’s a mechanical problem, involving muscles or nerves.
Gangrene.
Sustained swelling and distension of the gallbladder from chronic inflammation can eventually lead to tissue death. Dead tissues are at risk of bursting or tearing. A perforation in the gallbladder wall can put the rest of the abdominal cavity at risk of infection (peritonitis).
Gallbladder cancer.
Cancer of the gallbladder or bile ducts is rare but serious. Because symptoms of gallbladder cancer often don’t appear until the later stages,
gallbladder polyps (tumors or growths) are harmless. But if you have a polyp that’s larger than average, your healthcare provider may recommend removing it just to be on the safe side.
Cholangiopathy.
can result from a temporary infection, blockage or a progressive autoimmune disorder such as primary biliary cholangitis. Chronic cholangitis can result in scarring and narrowing of the bile ducts (biliary stricture). This can cause bile to back up into your gallbladder and liver.
- Osteoarthritis is a degenerative joint condition. It causes pain, swelling and stiffness, affecting a person’s ability to move freely.
Osteoarthritis is a degenerative disease that worsens over time, often resulting in chronic pain. Joint pain and stiffness can become severe enough to make ..
Osteoarthritis is the most common form of arthritis, affecting millions of people worldwide. It occurs when the protective cartilage that cushions the ends of the bones wears down over time.
- Affected joints might hurt during or after movement.
- Joint stiffness might be most noticeable upon awakening or after being inactive.
- Your joint might feel tender when you apply light pressure to or near it.
- Loss of flexibility. You might not be able to move your joint through its full range of motion.
- Grating sensation. You might feel a grating sensation when you use the joint, and you might hear popping or crackling.
- Bone spurs. These extra bits of bone, which feel like hard lumps, can form around the affected joint.
- This might be caused by soft tissue inflammation around the joint.
Bone spurs on spine
In osteoarthritis of the spine, disks narrow and bone spurs form.

-
Osteoarthritis of the hip
The hip joint shown on the left side of the image is normal, but the hip joint shown on the right side of the image shows deterioration of cartilage and the formation of bone spurs due to osteoarthritis.
Sleep apnea is a sleep-related breathing disorder in which repetitive pauses in breathing, periods of shallow breathing, or collapse of the upper airway during sleep results in poor ventilation and sleep disruption. Each pause in breathing can last for a few seconds to a few minutes and occurs many times a nigh
Sleep apnea is a serious sleep disorder that happens when your breathing stops and starts while you’re asleep. If it goes untreated, it can cause loud snoring, daytime tiredness, or more serious problems like heart trouble or high blood pressure.
- Snore much more loudly than those with regular snoring
- Pause for over 10 seconds while they breathe
- Take shallow breaths, gasp, or choke
- Be restless during sleep
Sleep Apnea Types
There are three types of sleep apnea:
Obstructive sleep apnea.
This usually happens because the soft tissue at the back of your throat collapses when the muscles in your face and neck relax while you sleep. During these episodes, your diaphragm and chest muscles must work harder than normal to open your airways. You may start to breathe with loud gasps, and your body may jerk. This can affect your sleep, lower the flow of oxygen to your vital organs, and lead to abnormal heart rhythms.
Central sleep apnea.
It’s related to the function of your central nervous system. This type most often affects people with neuromuscular disease such as amyotrophic lateral sclerosis (ALS, or Lou Gehrig’s disease), those who’ve had a stroke, or those who have heart failure or other forms of heart, kidney, or lung disease.
Complex sleep apnea syndrome. With this condition, you have a combination of obstructive and central sleep apnea. When you have the obstructive type but it turns into the central type after you get treatment, that’s called treatment-emergent central sleep apnea.
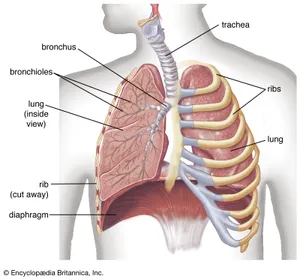
- Respiratory diseases, or lung diseases, are pathological conditions affecting the organs and tissues that make gas exchange difficult in air-breathing animals
The symptoms of lung disease are relatively few. Cough is a particularly important sign of all diseases that affect any part of the bronchial tree. A cough productive of sputum is the most important manifestation of inflammatory or malignant diseases of the major airways, of which bronchitis is a common example. In severe bronchitis the mucous glands lining the bronchi enlarge greatly, and, commonly, 30 to 60 ml of sputum are produced in a 24-hour period, particularly in the first two hours after awakening in the morning. An irritative cough without sputum may be caused by extension of malignant disease to the bronchial tree from nearby organs. The presence of blood in the sputum (hemoptysis) is an important sign that should never be disregarded. Although it may result simply from an exacerbation of an existing infection, it may also indicate the presence of inflammation, capillary damage, or a tumor.
The second most important symptom of lung disease is dyspnea, or shortness of breath. This sensation, of complex origin, may arise acutely, as when a foreign body is inhaled into the trachea, or with the onset of a severe attack of asthma. More often, it is insidious in onset and slowly progressive.
Chest pain may be an early symptom of lung disease, but it is most often associated with an attack of pneumonia, in which case it is due to an inflammation of the pleura that follows the onset of the pneumonic process.
To these major symptoms of lung disease—coughing, dyspnea, and chest pain—may be added several others. A wheeziness in the chest may be heard. This is caused by narrowing of the airways, such as occurs in asthma. Some diseases of the lung are associated with the swelling of the fingertips (and, rarely, of the toes) called “clubbing.” Clubbing may be a feature of bronchiectasis (chronic inflammation and dilation of the major airways)
lungs working Endometriosis affects roughly 10% (190 million) of reproductive age women and girls globally. It is a chronic disease associated with severe, life-impacting pain during periods, sexual intercourse, bowel movements and/or urination, chronic pelvic pain, abdominal bloating, nausea, fatigue, and sometimes depression, anxiety, and infertility. There is currently no known cure for endometriosis and treatment is usually aimed at controlling symptoms. Access to early diagnosis and effective treatment of endometriosis is important, but is limited in many settings, including in low- and middle-income countries. Endometriosis is a disease in which tissue similar to the lining of the uterus grows outside the uterus. It can cause severe pain in the pelvis and make it harder to get pregnant. Endometriosis can start at a person’s first menstrual period and last until menopause.
With endometriosis, tissue similar to the lining of the uterus grows outside the uterus. This leads to inflammation and scar tissue forming in the pelvic region and (rarely) elsewhere in the body. superficial endometriosis found mainly on the pelvic peritoneum
- cystic ovarian endometriosis (endometrioma) found in the ovaries
- deep endometriosis found in the recto-vaginal septum, bladder, and bowel
- in rare cases, endometriosis has also been found outside the pelvis.
Symptoms
Some people with endometriosis don’t have any symptoms. For those who do, a common symptom is pain in the lower part of the belly (pelvis). Pain may be most noticeable:
- during a period
- during or after sex
- when urinating or defecating.
Some people also experience:
- chronic pelvic pain
- heavy bleeding during periods or between periods
- trouble getting pregnant
- bloating or nausea
- fatigue
- depression or anxiety.
- Dyslipidemia is a metabolic disorder characterized by abnormally high or low amounts of any or all lipids or lipoproteins in the blood.
-
Lipids, such as cholesterol or triglycerides, are absorbed from the intestines and carried throughout the body via lipoproteins for energy, steroid production, or bile acid formation. Major contributors to these pathways are cholesterol, low-density lipoprotein (LDL) cholesterol, triglycerides, and high-density lipoprotein (HDL). An imbalance of any of these factors, either from organic or nonorganic causes, can lead to dyslipidemia.
-
Hyperlipidemia, also known as dyslipidemia or high cholesterol, means you have too many lipids (fats) in your blood. Your liver creates cholesterol to help you digest food and make things like hormones. But you also eat cholesterol in foods from the meat and dairy aisles.
Hyperlipidemia, also known as dyslipidemia or high cholesterol, means you have too many lipids (fats) in your blood. Your liver creates cholesterol to help you digest food and make things like hormones. But you also eat cholesterol in foods from the meat and dairy aisles. As your liver can make as much cholesterol as you need, the cholesterol in foods you eat is extra.
 Breast cancer is a disease in which abnormal breast cells grow out of control and form tumors. If left unchecked, the tumors can spread throughout the body and become fatal.
Breast cancer is a disease in which abnormal breast cells grow out of control and form tumors. If left unchecked, the tumors can spread throughout the body and become fatal.Breast cancer cells begin inside the milk ducts and/or the milk-producing lobules of the breast. The earliest form (in situ) is not life-threatening and can be detected in early stages. Cancer cells can spread into nearby breast tissue (invasion). This creates tumors that cause lumps or thickening.
Invasive cancers can spread to nearby lymph nodes or other organs (metastasize). Metastasis can be life-threatening and fatal.
Breast cancer can have combinations of symptoms, especially when it is more advanced. Symptoms of breast cancer can include:
A breast lump or thickening, often without pain
Change in size, shape or appearance of the breast
Dimpling, redness, pitting or other changes in the skin
Change in nipple appearance or the skin surrounding the nipple (areola)
- Abnormal or bloody fluid from the nipple.
- Prostate cancer is the uncontrolled growth of cells in the prostate, a gland in the male reproductive system below the bladder. Abnormal growth of prostate tissue is usually detected through screening tests, typically blood tests that check for prostate-specific antigen levels.
Almost all prostate cancers are adenocarcinomas. These cancers develop from the gland cells in the prostate (the cells that make the prostate fluid that is added to the semen).
Other types of cancer that can start in the prostate include:
- Small cell carcinoma (small cell neuroendocrine carcinoma)
- Other neuroendocrine tumors (including large cell carcinoma)
- Transitional cell carcinoma
- Sarcomas

Many cases of colon cancer have no symptoms. If there are symptoms, the following may indicate colon cancer: Abdominal pain and tenderness in the lower abdomen.
Colorectal cancer is cancer that starts in the large intestine (colon) or the rectum (end of the colon). It is also sometimes simply called colon cancer.
Blood in the stool
Diarrhea, constipation, or other change in bowel habits
Narrow stools
Weight loss with no known reason
You have a higher risk for colorectal cancer
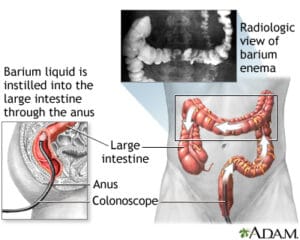
- Are age 45 or older
- Drink alcohol
- Smoke tobacco
- Are overweight or have obesity
- Are African American or of eastern European descent
- Eat a lot of red or processed meats
- Eat a low-fiber and high-fat diet
- Have a diet low in fruits and vegetables
- Have colorectal polyps
- Have inflammatory bowel disease (Crohn disease or ulcerative colitis)
- Have a family history of colorectal cancer